Imagining a Biorisk-Free World: An Outline of the Biosecurity Solution Space
Introduction to Biosecurity Series - Part V
This article was written as part of a period of self-teaching and was used to facilitate my learning. I can’t promise it’s insightful, original, or even accurate. However, I can promise that my next article will be a little better.
____________________________________________________________________________
From the risk of a terrorist organisation operating its own bioweapons program to the emergence of superbugs due to antimicrobial resistance, I previously laid out the broad spectrum of biorisk, from the emergence of a pathogen to the downstream effects posed by an outbreak.
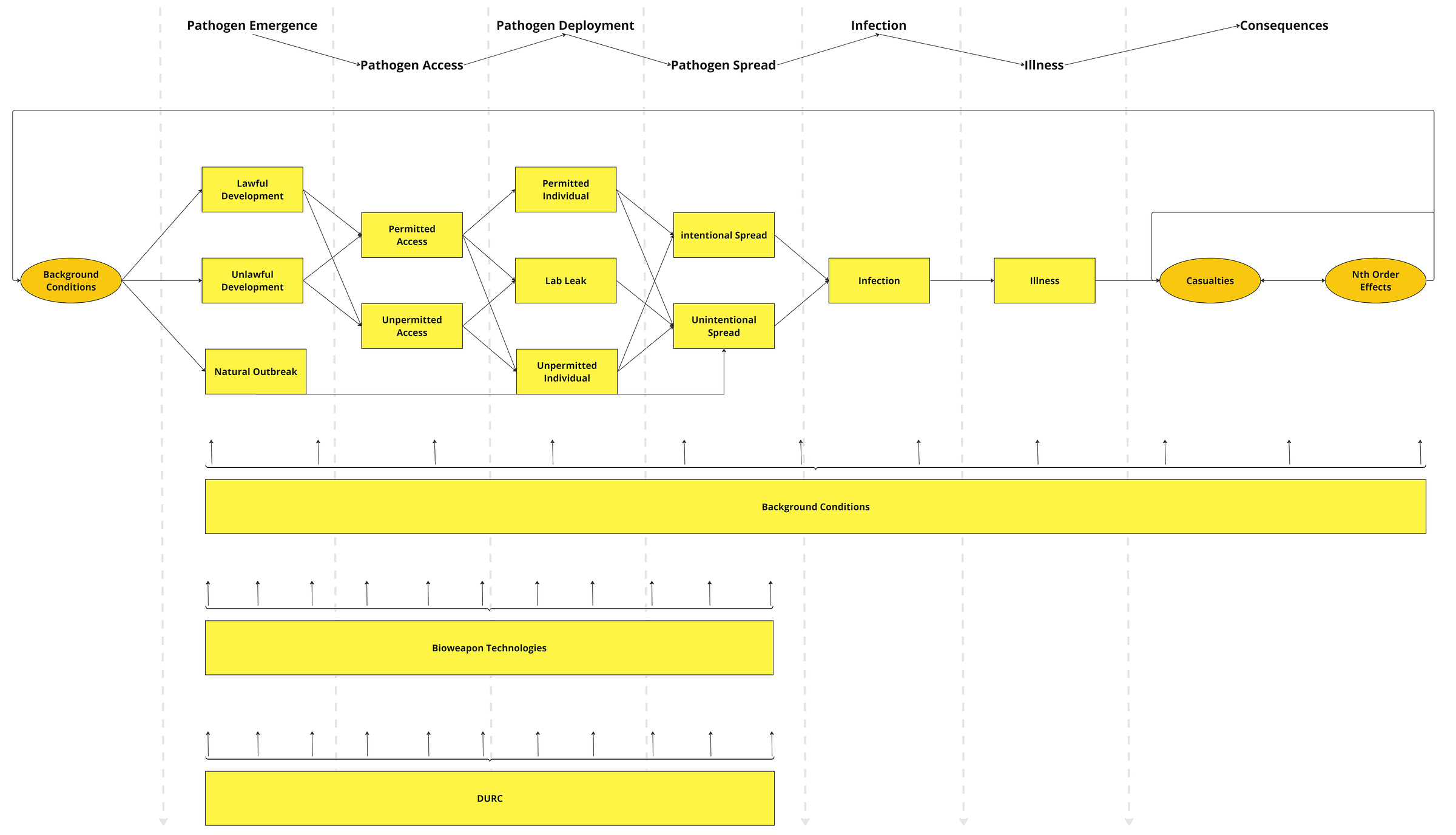
However, a broad spectrum of risks should also mean a wide spectrum of countermeasures - and when it comes to dealing with biorisk, we are spoilt for choice. For a top-down understanding of the biosecurity landscape, we can use my ‘Handgun Model of Biorisk’ as a starting point.
In particular, we can conceptualise all biosecurity efforts as attempting to prevent the emergence, spread, deployment, or spread of a pathogen; mitigate the infections, illness, and adverse nth-order effects of an outbreak, or create favourable background conditions.
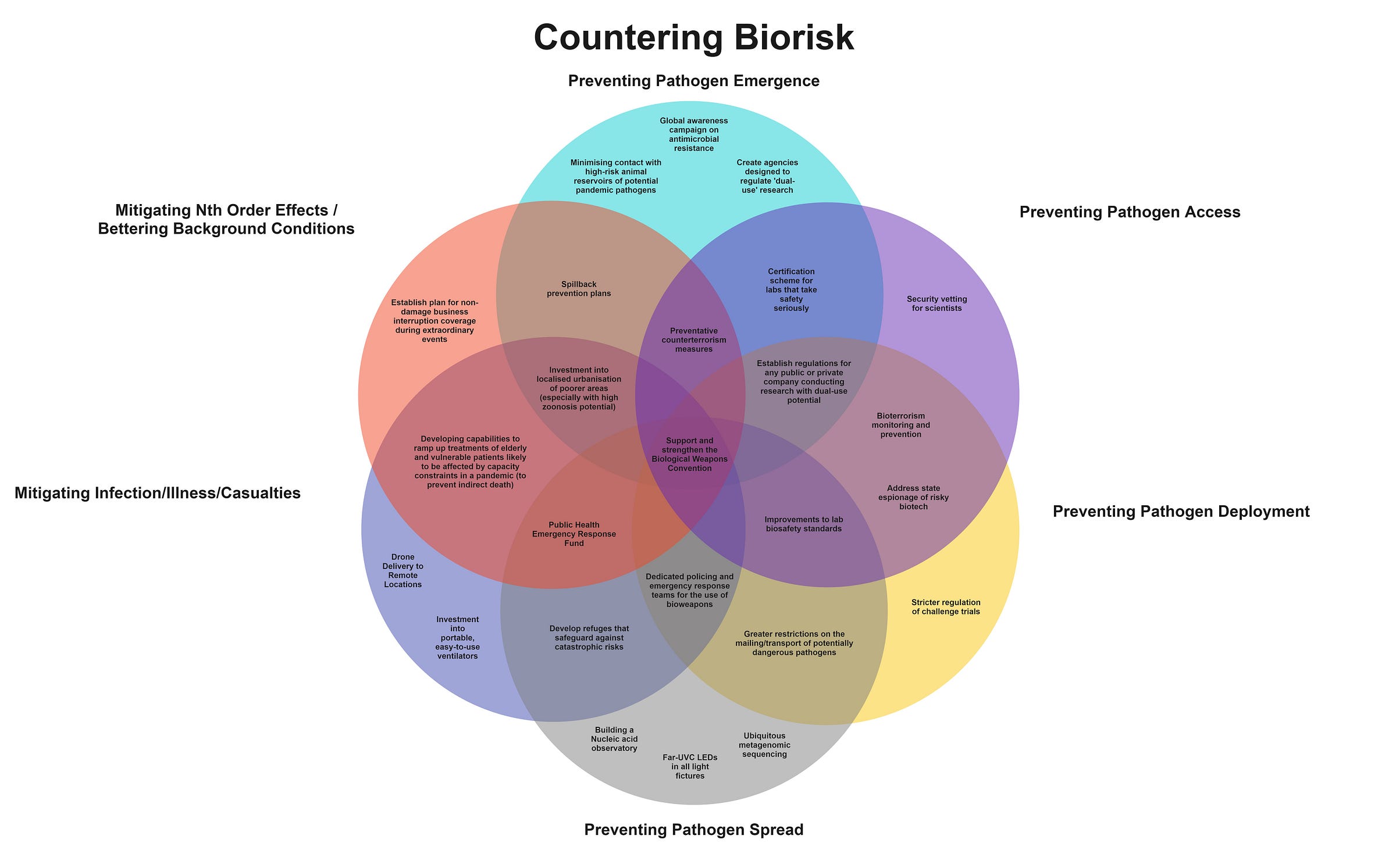
However, unlike the steps to an outbreak, these categorisations are not mutually exclusive. For example, interventions may simultaneously prevent the emergence of and access to a dangerous pathogen. Or, they may attempt to mitigate casualties and create favourable nth-order effects simultaneously. Or, as is the case for certain governance interventions, they may attempt to decrease biorisk across all these domains.
Thus, it helps not only to think of addressing biosecurity as a complex, interdependent, and multi-faceted web of prevention, but as an even broader tangled web of policies, programs, initiatives, and norms to prevent outbreaks; address them when they emerge, and ensure the world is positioned to keep the risk of an outbreak as low as possible.
In other words, a more representative picture is captured by the following Venn diagram:
Future blog posts will explore many of these interventions in more detail. However, in this post, I briefly aim to get across the breadth of the solution space for biosecurity by outlining what a biorisk-free world might look like.
1. A Perfect Calm
What does a world look like in which we have little reason to even worry about an outbreak in the first place?
On natural outbreaks, it looks like the absence of factors that makes them substantially more likely. Namely, less rapid changes in land use; limited human-animal contact, slowed climate change, and strong public healthcare systems worldwide. This state of affairs wouldn't arise naturally. In this world, advocacy efforts to reduce climate change successfully influenced policy (e.g. commitments to reduce emissions), and technologies to reduce climate change (such as solar panels) were successfully developed and proliferated at pace. We successfully managed to prevent the proliferation of animal reservoirs, and nations committed to expanding their foreign aid program to assist global health.
In this world, we also do not worry about the threat of human-caused outbreaks (accidental or intentional) because there is no conflict between states; a lack of terrorist organisations interested in developing bioweapons, and very few BSL-4 labs regularly experimenting with dangerous pathogens around the world. Similarly, we did not fall into this world by chance. International peacebuilding is a profoundly complex process that involves addressing factors from local hostilities to the degree of international commitment and cannot be done without gradually entrenching norms of security. Moreover, preventing domestic terrorism requires a comprehensive strategy and is much more difficult in countries lacking appropriate governance and enforcement mechanisms. Thus, in this world, universal state-building and development efforts succeeded, ensuring nation-states everywhere can prevent the emergence of dangerous terrorist groups.
2. The Web of Prevention
Of course, we do not live in a world without conflict, terrorist organisations, or the absence of human-to-animal contact. So how can we prevent a dangerous pathogen's emergence, access, and deployment? We would do this by deploying an effective web of prevention.
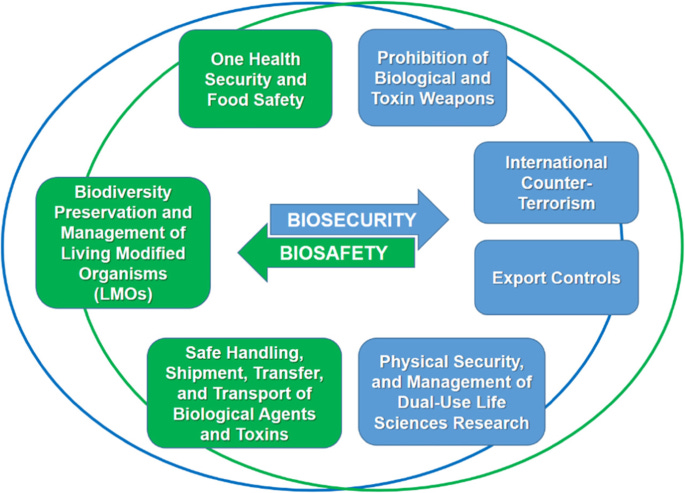
A “web of prevention” is an important concept in biosecurity, encapsulating the multi-pronged approach required to limit the odds of an outbreak in the first place. It refers to “the set of complementary and mutually reinforcing policies, regulations and measures that need to be in place to counter the development and use of any form of biological and toxin weapons and guarantee that the life sciences are used only for peaceful purposes”.
So what does a world where we have successfully implemented a web of prevention look like?
For one, it looks like strict controls around technology and research that may lead to a dangerous pathogen emerging in the first place. An ethics committee regulates dual-use research of concern. For example, dual-use; access to DNA synthesis materials requires cryptographic screening; the sale of antibiotics is regulated by an international body (to limit the chance of bacteria developing antimicrobial resistance), and an international body exists to track the number and safety measures at animal reservoirs worldwide to limit the chances of zoonotic transmission.
As discussed previously, much of the threat of a bioweapon being released is the product of rapid advances in synthetic biology. In turn, strong norms have been built in the academic community to promote differential technological development - the acceleration of technologies that promote biosecurity and the slow-down of technology that poses greater dual-use risk. This includes journal review processes considering dual-use threats; diverting funding towards robustly promising biosecurity interventions, and promoting differential technological development as a worthwhile norm at scientific conferences.
On top of this, the Biological Weapons Convention - in this world signed by all countries (unlike the status quo) - not only represents a global consensus by states not to develop bioweapons, but effective enforcement, verification, and accountability mechanisms exist to ensure states cannot break this agreement.
Access to dangerous pathogens is greatly limited by robust biosafety standards that include security vetting for scientists; effective and coordinated screening that involves information sharing about potentially dangerous individuals, and export controls preventing dangerous materials from crossing the border. In addition, international counterterrorism efforts are well-developed, including information sharing between states; surveillance of known terrorist factions, and effective international policing via cooperation through INTERPOL.
Biosafety standards are crucial to preventing the illicit deployment of dangerous pathogens. This includes stringent national regulation concerning challenge trials and measures to prevent the mailing of dangerous pathogens (as in the 2001 anthrax attacks). In addition, a reporting system exists to identify a lab-acquired infection with epidemic potential immediately, and appropriate countermeasures against lab leaks exist both as lab biosafety standards and local policy.
3. A Global Immune System
If we cannot stop a pathogen from emerging in the first place, it is important to detect and defend against pathogens. The world where we can successfully do this looks like having an effective global immune system against pathogens.
The potential measures here are plentiful. At a global and national level, it involves rapid early detection through technologies such as metagenomic sequencing and multiplexed PCR assays, allowing for the rapid diagnosis of any known pathogen - and, in turn, the immediate spotting of an unknown pathogen. In addition, a global nucleic acid observatory is built to sample wastewater for the presence of dangerous pathogens routinely. Countries build digital pathogen surveillance networks at hospitals that include multiplexed point-of-person diagnostics that they can instantly share with the relevant authorities when they detect a potential pandemic pathogen.
Once we have detected the pathogen, developing and using vaccines to mitigate further spread is crucial. In this world, we do this by investing in flexible and scalable manufacturing of pharmaceuticals, needle-free methods of drug administration, and vaccine platform technologies - all coordinated by a specialised pandemic response unit.
We don’t only rely on vaccines to limit the spread, however. High-efficacy sterilisation is cheap and widely used; far-UVC lights are ubiquitous and kill airborne pathogens in nearly every room. High-quality personal protective equipment (PPE) is developed and then rapidly dispersed at the point of detecting an outbreak. Quarantining and social distancing are enforced globally - but years of education have created a high-trust environment where measures are followed.
We do not just rely on these methods on a global level, but preventative measures are widespread at home too. Individual diagnostic tests, powered air-purifying respirators, far-UVC lightbulbs, and cheap universal vaccines are already widespread at the point of detection.
4. Healthcare for All
On top of preventing the spread of these pathogens, several measures are in place to adequately treat patients - all enforced by cooperation between the government, the specialised pandemic response unit, and a National Public Health Data system.
This includes needle-free drugs; broad-spectrum antiviral agents; and rapid pop-up hospitals. For particularly catastrophic pathogens, telemedicine is widespread; a drone delivery system of medicines exists, and for-profit companies have already been paid to lend their manufacturing capabilities to developing medicines quickly. If things are terrible, hundreds of airtight refuges are dispersed throughout major cities that individuals can flock to during an outbreak.
Effectively, a global healthcare system exists that involves a network of labs, hospitals, pharmaceutical companies, and governments to coordinate the delivery of all of the above.
5. Holistic Mitigation
Not only is there coordination to deal with outbreaks directly, but institutions and governments are aware of the many indirect effects pandemics can have. In turn, plenty of mechanisms exist to combat these.
States have already built plans for non-damage business interruption coverage during extraordinary events, which includes economic reserves for biorisks; regulations requiring several industries to have the tools to facilitate work from home, and measures in place to ensure those most directly affected - e.g. individuals in hospitality - can receive economic support, training, and the ability to reskill as needed during the pandemic.
The electrical grid is kept functional, even amidst the potential for pandemics to make this difficult, through appropriate automation, pandemic-relevant policies, and specialised PPE. Aware that indirect deaths form a considerable proportion of pandemic-related casualties, measures exist to ensure the elderly and most vulnerable in the population can continue receiving medical treatment for unrelated ailments throughout - i.e. by ramping up funding for hospitals likely to be stretched or creating pop-up hospitals for individuals who need to continue receiving specialised care but are vulnerable to a pandemic.
Finally, there is an appropriate international effort to regulate travel and appropriate expansionary policy in the aftermath of the pandemic to prevent further casualties through a severe economic recession.
A lot has been said of the importance of international coordination in facilitating all of these measures, and the institutional arrangement is a considerable part of making this work. In this world, a global Public Health Emergency Fund likely exists; instantaneous sharing of national public health data; scientist exchange programs; a program to transport physicians to poorer states as needed; programs to reskill practising medical professionals to deal with the specific threat, and reform to the Biological Weapons Convention to create the capacity for appropriate countermeasures (as right now, the BWC gets funded on the order of only ~ $1.5m a year). The world where we can pull all of the above is one with considerably more interstate cooperation.
6. Conclusion: How Do We Get Here?
If this were the world we lived in, COVID-19 would not remain a leading cause of death in many parts of the world. However, it is not. So how do we get here?
One obvious answer is the advocacy for, and implementation of, the above policies. Examples of such proposals include The Apollo Program for Biodefense and Kevin Esvelt’s Delay, Detect, Defend agenda for biosecurity.
However, there are several possible community-building efforts that can grow the community of individuals interested in biosecurity. This includes competitions on synthetic biology and genetic attribution; fellowships for biosecurity, and increasing public awareness of issues such as antimicrobial resistance.
Future posts will give more detailed explorations of how we can move towards a biosecure world. However, for now, the point of this article is to demonstrate that this will not occur via a singular silver bullet intervention. The biosecurity solution space is vast, and this article has only scratched the surface. A multi-pronged, end-to-end, and varied approach involving individuals, firms, states, and international bodies addressing all parts of the biorisk threat landscape is essential to ensuring we are fully defended from biorisks.